Syphilis is a complex infectious disease caused by a bacteria named Treponema pallidum. Transmission occurs mostly during sexual contact (including oral sex), through minor skin or mucosal lesions; sites of inoculation are usually intrarectal, perianal, or oral. It may be anywhere on the body, also, syphilis can probably penetrate intact mucous membranes, or it may enter through a break in the epidermis. The risk of acquiring syphilis after unprotected sex with an individual with infectious syphilis is approximately 30-50%. Rarely, through nonsexual contact like blood transfusion or via the placenta from mother to fetus (congenital syphilis) syphilis can be transmitted. Congenital syphilis happens from the beginning of 10th to 15th week of gestation. Some of the infected fetuses die, and miscarriages result; others are still born at term. Others born live but develop the sign of congenital syphilis in childhood: interstitial keratitis, Hutchinson’s teeth, saddle-nose, periostitis, and a variety of central nervous system anomalies. That is why syphilis test is a must for intending mothers. Adequate treatment of the mother during pregnancy prevents congenital syphilis.
Syphilis infection is categorized into 3;
- Primary syphilis: this is categorized by the appearance of a painless papule also known as chancre (an ulcer with a clean, hard base) at the point of infection, usually the genital or oral site. This happens between 2-10 weeks after infection, as infection spreads through nearby lymph nodes and then reach the blood stream. The primary lesions always heal spontaneously.

syphilis primary chancre scale
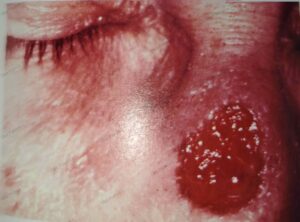
- Secondary syphilis: if the primary form is untreated, this may result in the secondary form from 20 to 60 days after infection, resulting in a maculopapular rash which is red to reddish brown in color with common palmoplantar involvement. There may be a scarring alopecia, ulceration of mucous membranes and characteristic pale papule (condylomas) in the anogenital region, axilla and mouth (flexures). Condylomas are white grey and, due to their presence in flexures, tend to be moist. Systemic symptoms include fever, lethargy, myalgia, and arthralgia. There may also be syphilitic meningitis, chorioretinitis, hepatitis, nephritis, or periostitis. The secondary lesions also subside spontaneously.

perianal condyloma in secondary syphilis
- Tertiary syphilis: this may develop approximately 3-5 years after infection. Tuberous syphilids with grouped red-brown papules occur on skin. Such lesions develop with central regression and atrophy. Associated peripheral progression results in serpiginous morphology. This developed granulomatous lesions (gummas), may be localized on the forehead, scalp, lips, tongue, genitals, or any part of the body. Morphologically, the gummas are various shades of red and may ulcerate and heal with extensive scarring.
gumma of the nose due to long-standing syphilis
TREATMENT
The treatment of choice is penicillin, but allergic individuals respond to erythromycin of tetracyclines. In neuro=syphilis, same therapy is treatment of gonorrhea is thought to cure incubating syphilis. Prolonged follow-up is essential. In neuro-syphilis, treponemes occasionally survive such treatment. Severe neurologic relapses of treated syphilis have occurred in patients with acquired immunodeficiency syndrome (AIDS) who are infected with both HIV and T pallidum. A typical Jarish-Herxheimer reaction may occur within hours after treatment is begun. It is due to release of toxic products from dying or killed spirochetes.
LABORATORY TESTS
- Microscopy using dark field microscopic examination.
- Serologic tests for syphilis which includes (a) nontreponemal antigen tests like venereal disease research laboratory (VDRL), rapid plasma reagin (RPR), (b) Treponema antibody tests like treponema pallidum hemagglutination (TPHA), treponema pallidum particle agglutination (TPPA), (c) Enzyme immunoassay (EIA), chemiluminescence (CIA), (d) rapid treponemal tests.
- Polymerase chain reaction (PCR)
- Cerebrospinal fluid examination
PREVENTION
Avoidance of sexual contact is the only completely reliable method of prevention but is an impractical public health measure. Condoms are effective but protect covered areas only. Screen every 6-12 months for syphilis. High risk individuals (those with multiple encounters with anonymous partner or drug users) should be screened every 3 -6 months. Pregnant women should be screened at the first antenatal visit and again in the third trimester, if there is high risk of infection. Indicator of high risk includes poverty, sex work, illicit drug use, history of other sexually transmitted diseases and so on. Patients treated for other sexually transmitted infections should also be tested for syphilis.
REERENCE
CURRENT Medical Diagnosis and Treatment 2013 Papadakis et. al.
Jawetz, Melnick, & Adelberg’s Medical Microbiology 23rd edition.
MANSON’S TROPICAL DISEASES 22ND EDITION